Patient With Swallowing Disorder Gets New Lease On Life
Swallowing food – something many of us don’t ever think of – is constantly on the mind of Jay Anderson. The 43-year-old from Plattsburgh has had to worry about it ever since he began treatment for cancer on his tonsil, tongue and throat about a year ago. Now, thanks to a new device that’s the only one of its kind in the University of Vermont Health Network, Anderson enjoys something he hasn’t experienced in quite a while: confidence to eat and drink.
“There have been a lot of dark days for me,” Anderson recalls. “I’ve had an aneurysm. They’ve had to go in my throat and do two different surgeries. Plus, I’ve been intubated twice and they had to work with me to get my jaw to open up. I’ve been through quite a few things, and the swallowing part has been really difficult for me.”
Dysphagia (difficulty in swallowing) is a common side effect of radiation therapy, and it became a problem for Anderson after undergoing three dozen rounds of radiation and several rounds of chemotherapy. It became difficult for him to eat or drink, with food and liquids getting stuck in his airway, known as aspiration. Choking, pneumonia, and lung infections are just some of the issues that can affect the quality of life for patients suffering from dysphagia.
As a result, Anderson had to rely on a feeding tube. He lost nearly 100 pounds. Family and friends did all they could to support him, and he noticed a change in their eating habits.
Times like Thanksgiving and Christmas were tough. People kind of shied away from eating [in front of me] when I couldn’t. It’s different, being the odd man out. But I’d tell everybody, you know, have a normal day. Don’t worry about me. And they always treated me with nothing but respect.
Jay Anderson
A New System Changes Everything
As Anderson underwent cancer treatments and swallowing challenges, UVM Health Network-Champlain Valley Physicians Hospital was able to acquire a new system called Flexible Endoscopic Evaluation of Swallow (FEES), making it the first hospital in the region with a device that can make a big difference for patients like Anderson.
“What’s great about this is we can help a lot of people across northern New York and Vermont who wouldn’t have access to this amazing system,” says Anthony Lewis, a speech language pathologist at the hospital. “And this isn’t just for patients with cancer. Dysphagia affects people with a history of stroke, neuromuscular diseases like Parkinson’s or ALS and muscular dystrophies.”
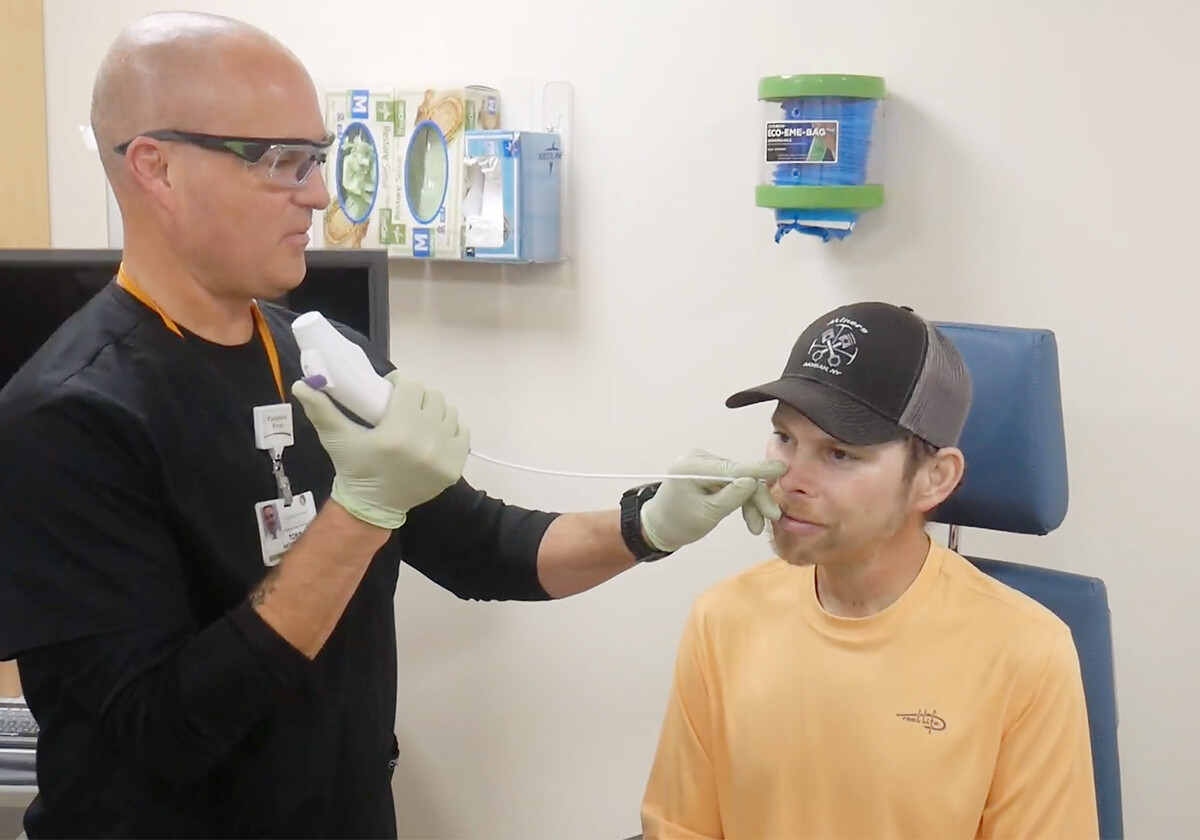
The system consists of an endoscope, which is a flexible tube about the size of a shoelace, with a tiny, high-definition camera and light on its tip. The endoscope is inserted through the patient’s nostril and into the throat, and the camera sends live pictures back to a video screen.
“It’s not as bad as you think,” Lewis offers. “When we first got the system, we scoped ourselves multiple times. We lubricate the scope, and there’s a certain amount of skill involved that came with practice before we used it on patients. We’re very careful to not touch anything that could cause adverse reactions.”
“I have a pretty intense gag reflex, but he [Lewis] just nails it. He doesn’t touch anything that would cause that,” says Anderson, who was one of the first patients to undergo a FEES study at Champlain Valley Physicians Hospital (CVPH).
Another important piece of the puzzle is the chair used during the study, which was purchased with donations from The Foundation of CVPH. It is crucial for positioning patients as the exam is happening, providing safety and comfort for both the speech language pathologist and the person in the chair.
“The cool thing about this chair is that it’s very comfortable and it’s very stable. That helps the patients feel like they’re safe and secure during the study, which makes them relax, allowing us to get better data,” Lewis explains.
“It makes me feel like I’m on the Starship Enterprise, ready to take off,” Anderson jokes. “Seriously though, they can adjust it so I’m comfortable. It’s a perfect chair.”
Lewis adds that the chair’s ergonomic, fully adjustable seating and positioning options offer him and his colleagues conducting the exam more comfort, improving observation and diagnostic ability. It accommodates a wide range of body types and sizes. And the chair can be positioned quickly to allow the patient to lie back with feet elevated should they feel faint, a possible side effect of the test.
Getting an Inside View
Once the patient is comfortably positioned and the speech language pathologist inserts the endoscope, the patient is provided a variety of foods and liquids to swallow. That’s when Lewis can really get a good idea of what’s leading to the swallowing problems.
“We’re looking for how efficiently the patient is swallowing. Are they able to swallow safely? We can really see the root cause of the problem in real time, as it’s happening. That’s the diagnostic capability.”
“Therapeutically, it allows us to offer suggestions to the patient, like ‘tuck your chin when you swallow,’ or ‘rotate your head,” says Lewis. “The position of their head and neck can help facilitate more efficient swallowing. And then we can see whether or not what we recommend is actually working, and adjust if need be.”
Lewis also notes that the video system is a great educational tool for patients.
“We can have the patient watch what’s going on inside of their throat when they swallow. And that’s helpful for them to understand what causes a certain sensation or what might actually be the most effective position to swallow in,” he says.
I couldn’t tell you the amount of things I’ve learned from Day One until now. It’s amazing. Now I know why I can get a very faint cough for a while if I can’t get something solid to completely go down. And I know that holding my head up versus down makes it easier for me. Just that simple thing made a big difference.
Jay Anderson
FEES Pays Off
The benefits of the FEES studies are enormous.
“I think it gave Jay some confidence, knowing that he was safer to eat than he felt, and therefore he was able to eat and drink more by mouth and rely less on the feeding tube,” Lewis points out.
“It almost makes me feel normal again. I used to have a hard time putting one M&M in my mouth and manipulating it. Now, I can almost make that thing dance! I’ve come a long way,” Anderson says with a big smile on his face.
Anderson credits the FEES studies with helping him come out of the dark days he was experiencing. Ice cream has become a favorite treat.
“You can eat an ice cream sandwich faster than anyone I’ve ever seen,” Lewis says to Anderson.
“Yes, ice cream is my friend,” Anderson replies. “When someone says eat as much ice cream as you want, you should see my freezer!”
Anderson is spending as much time with his family as he can, going hunting and fishing with his nephews and nieces. “I helped my nephew wire some lights on his four wheeler,” he says. “You know, if it’s got wheels, we’re probably involved somehow.”
He’s also not taking anything for granted.
“In order to do everything with the chemo and radiation, I had to quit smoking. And I did it. It’s been over 7 months. So I remember walking to my mom’s house, and she had made apple crumb. I could smell that before I even opened the front door, because my nose came back. Things smell so good now. Like the blossoms on the trees. You don’t realize what you’ve lost until it’s gone. I’m just glad I’m getting it all back,” Anderson says.
At the moment, Anderson is cancer free and working hard to gain some of the weight back that he lost from his trouble swallowing. He says he’s incredibly thankful for all of the people who have worked to help him turn his life around after all that he’s been through.
“I can’t thank the oncology people at CVPH enough. Thank you to The Foundation for that chair that made it so comfortable going through the FEES exams to fix my swallowing problems.”
And I couldn’t have done any of this without my family and friends. This team of people who helped fill things out and made sure bills were paid on time, during a time I could barely keep my eyes open because I was so exhausted. So many people came to me and asked what they could do for me. I’ll always remember that.
Jay Anderson
