Embracing the Power of AI in Health Care

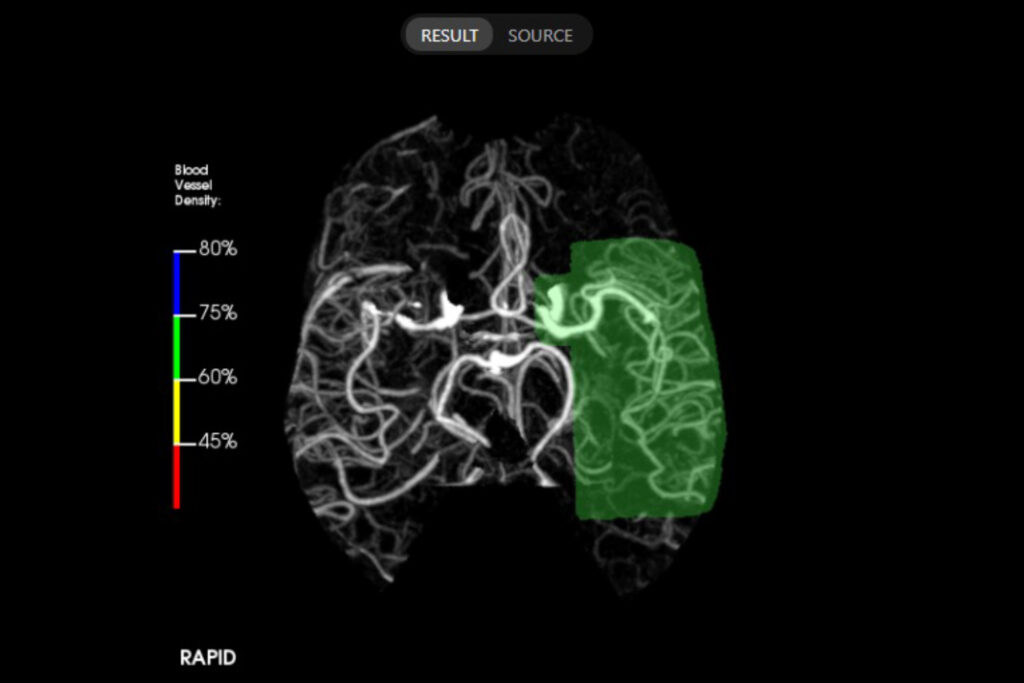
A disoriented patient arrives at Porter Medical Center’s 10-bed emergency department in Middlebury – part of the University of Vermont Health Network. After an initial assessment, a physician’s assistant orders a “Computed Tomography Angiogram” (CTA) – a special CT scan that assesses for blockage in an artery carrying blood to the brain. Seconds after the imaging is complete, an Artificial Intelligence (AI) program called “Rapid AI” reviews the results, determines that a stroke may be evolving and automatically notifies an on-call neurologist at the University of Vermont Medical Center who is a member of the 24/7 UVM Medical Center Stroke Team. The notification even highlights the area of the brain neurologists should focus on.
Sometimes we’re actually able to look at the image before a radiologist. If there is a clear issue that needs major intervention, the on-call neurologist gets the medical chopper on standby to bring the patient to UVM Medical Center for surgery and calls the ED provider to start an IV of ‘clot busting’ medications.
Christopher Commichau, MD, Director of the Stroke Team
Even if there isn’t an issue that requires such rapid intervention, when Porter Medical Center’s physician’s assistant requests a tele-stroke consult, a UVM Medical Center stroke specialist can review a scan and patient information before meeting virtually with the local provider and patient or family to create a care plan.
According to Dr. Commichau, the ability to do a CTA scan in addition to a traditional CT scan when stroke is suspected is a major advantage to UVM Health Network partners. “The ability to identify large vessel occlusions early on has made a significant difference for our patients, especially in smaller communities where access to this type of imaging was once limited. Our Network community hospitals are extremely advanced in that regard relative to others in New England. Clinically, it all means less waiting when patients have a condition where time-to-treatment matters.”
When Rapid AI was deployed in the UVM Health Network in 2018, it was considered a leading-edge technology that ensured equal access to top specialists who are based at the academic medical center – cutting critical time from testing to treatment.
Since then, UVM Health Network has brought on other cognitive computing models – many through its electronic medical record system, Epic. These models can identify patients who exhibit known risk factors and bring that information to the attention of medical providers. One such system identifies patients admitted to the hospital who are at a particularly elevated risk of sepsis – a life-threatening condition brought on by infection. These models are helpful in ensuring that all known risk factors are consistently reviewed, even in busy circumstances like the emergency department.
With the rise of natural language models and artificial intelligence – like Chat GPT – the UVM Health Network is preparing to begin implementing even more sophisticated AI software that promises to improve speed and accuracy of clinical documentation, reduce the staggering administrative burden faced by healthcare providers and improve patient care and population health.
Finding More Needles in the Same Haystack – Iodine
A major benefit to AI technology is its ability to analyze massive amounts of data swiftly and strategically. In August of 2023, the UVM Health Network implemented a natural-language and data-mining artificial intelligence program called Iodine that reviews inpatient medical records to identify potential diagnosis gaps.
Iodine reviews many points of data – clinical notes, test results, diagnoses and medications – and flags areas in which it believes additional documentation is needed. If for example, a patient tests positive for a condition, but the provider’s notes from the visit don’t specifically reference it, Iodine would flag the potential omission for further review by specialized nurses. Once reviewed, the doctor would receive a recommended chart revision for approval via an easy-to-use app on a mobile device.
According to UVM Health Network Associate Chief Medical Information Officer Justin Stinnett-Donnelly, MD, Iodine typically increases the number of chart reviews sent to providers by 20% to 40%.
Implementing this tool will not only result in substantial time savings for our doctors and advanced practice providers, but will also improve medical record and diagnostic accuracy.
Dr. Stinnett-Donnelly
Faster Charts for Patients, Less Burnout for Providers – Through Natural Language Processing
A major pain point for primary care providers is documentation and charting after a patient visit. Often, this task is delayed because of a physician’s busy daily schedule. Instead, it is performed after hours, often late at night, which can lead to exhaustion, burnout and turnover. Delayed documentation can also often result in an inaccurate picture of a patient’s condition and treatment and can cause confusion for the patient or other members of the care team.
The UVM Health Network plans to pilot a new tool that uses artificial intelligence natural language processing to transcribe and interpret entire interactions between healthcare providers and patients, generating progress notes from these conversations for a healthcare professional to quickly review and approve.
We hope this is going to improve everyone’s experience when it comes to documentation. Documentation puts an enormous amount of pressure on our healthcare providers. The less time they’re spending entering data, the more time they can spend with their patients, and that’s the whole reason they’re here.
Todd Young, Associate Vice President of Digital Health Services
AI Governance and Use Principles
At the core of the UVM Health Network’s Artificial Intelligence integration lies a robust framework of policies and principles governing its implementation. These strictures are centered on the knowledge that employees will demand tools that are available to perform their work more efficiently and guidelines are needed to ensure that appropriate tools are selected and implemented safely, equitably and responsibly.
AI has the ability to process vast amounts of data to gain valuable insights and efficiencies, but it is not yet at the point where it can or should replace clinical judgment. Additionally, since most AI tools use cloud-based computing to process information, precautions must be used to protect patient privacy.
“Our commitment lies in a thoughtful and responsible approach to AI,” says Douglas Gentile, Senior Vice President of Network Information Technology. “By addressing ethical concerns, ensuring data security, and promoting transparent governance, we’ve created a framework that safeguards patients and ensures that our teams use these tools to provide better care. Especially in clinical care, AI needs to be designed around the clinician as a complement to medical expertise. AI generates a draft or an alert, but an expert clinician needs to review the output and then take appropriate action.”
A Glimpse into the Future
Looking ahead, the UVM Health Network is committed to exploring new frontiers in AI application within the healthcare landscape. For instance, someday it may help improve patient communication or aid in the check-in process. One study even indicated that AI-generated responses to patient questions were perceived as more empathetic than those written by human healthcare providers.
Regardless of the specific application, AI will make the patient experience better by giving healthcare providers faster access to relevant data to make clinical decisions and empowering care teams to spend less time documenting and more time with patients.
I finished my neurology fellowship about 25 years ago and back then I never imagined tools like these,. Now it just seems like a natural evolution. This technology is just going to keep getting better and better.
Christopher Commichau, MD, Director of the Stroke Team
